Understanding Restless Leg Syndrome: Causes and Treatment
Are you experiencing restless legs at night? Do you find it difficult to get a good night’s sleep? Look no further! In this article, we will explore the causes and treatment options for Restless Leg Syndrome (RLS). At Vector Sleep Clinic, we understand the impact that sleep disorders can have on your overall well-being. With our licensed and insured clinic conveniently located in the heart of Rego Park, we offer comprehensive care to help you achieve restful nights and unlock the magic of rejuvenation. Don’t let sleep disorders affect your health or productivity any longer – read on to learn more about RLS and how we can assist you in finding a solution.
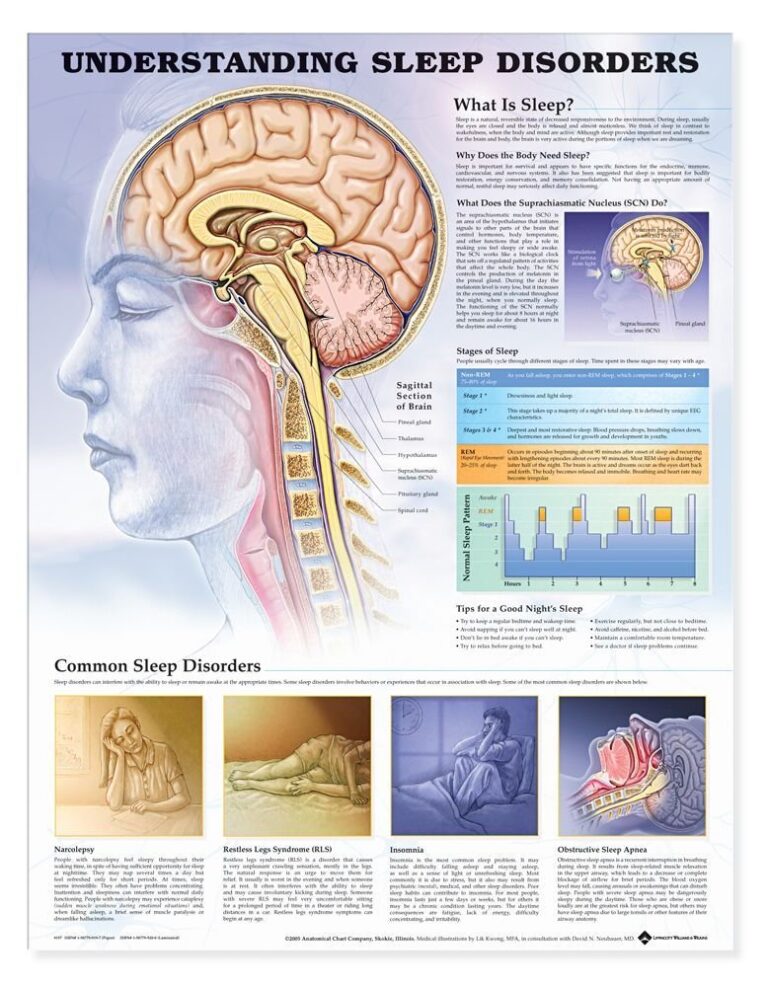
Understanding Restless Leg Syndrome
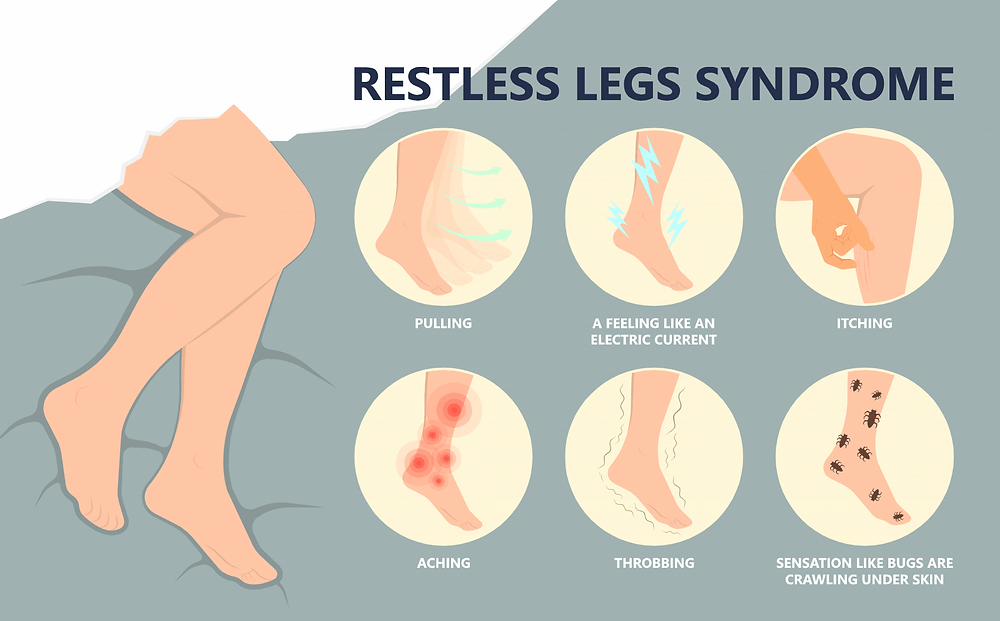
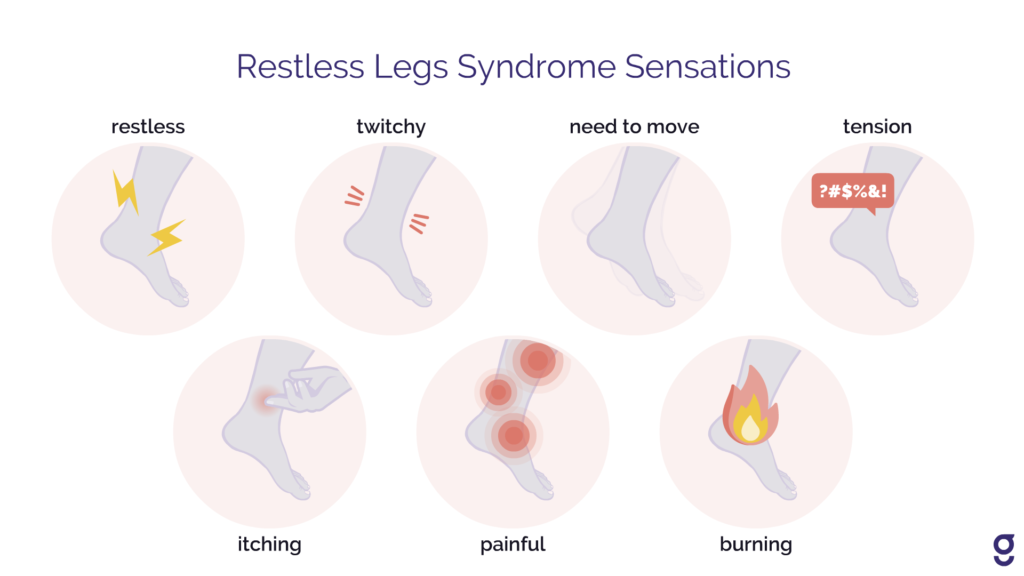
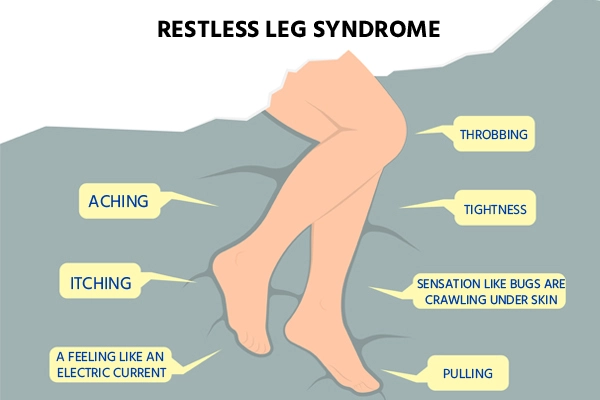
Restless Leg Syndrome (RLS) is a neurological disorder characterized by uncomfortable sensations and an irresistible urge to move the legs. This condition is often accompanied by an unpleasant tingling or crawling sensation, which is temporarily relieved by movement. RLS can significantly impact a person’s quality of life, particularly their ability to sleep peacefully.
Epidemiology: Who is affected?
RLS is a common condition, affecting approximately 5-10% of the population. It can occur at any age, but the prevalence tends to increase with age. Women are more frequently affected than men, and the symptoms often worsen during pregnancy.
Significance of RLS in overall health
While RLS itself is not life-threatening, its impact on overall health should not be underestimated. The disrupted sleep patterns caused by RLS can lead to excessive daytime sleepiness, reduced concentration, and impaired cognitive function. Additionally, studies have suggested a potential association between RLS and conditions such as cardiovascular disease and depression. Therefore, it is crucial to understand and manage RLS effectively.
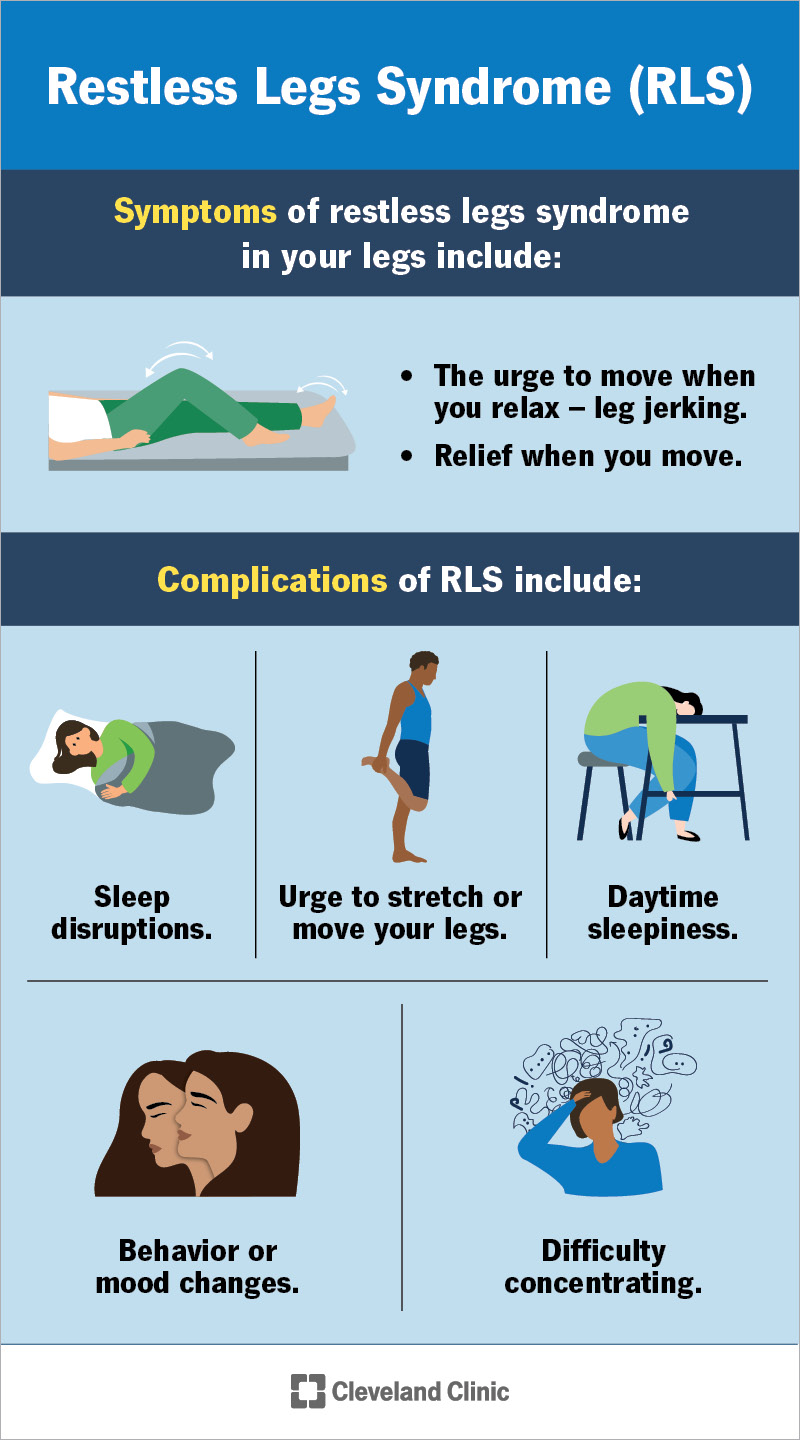
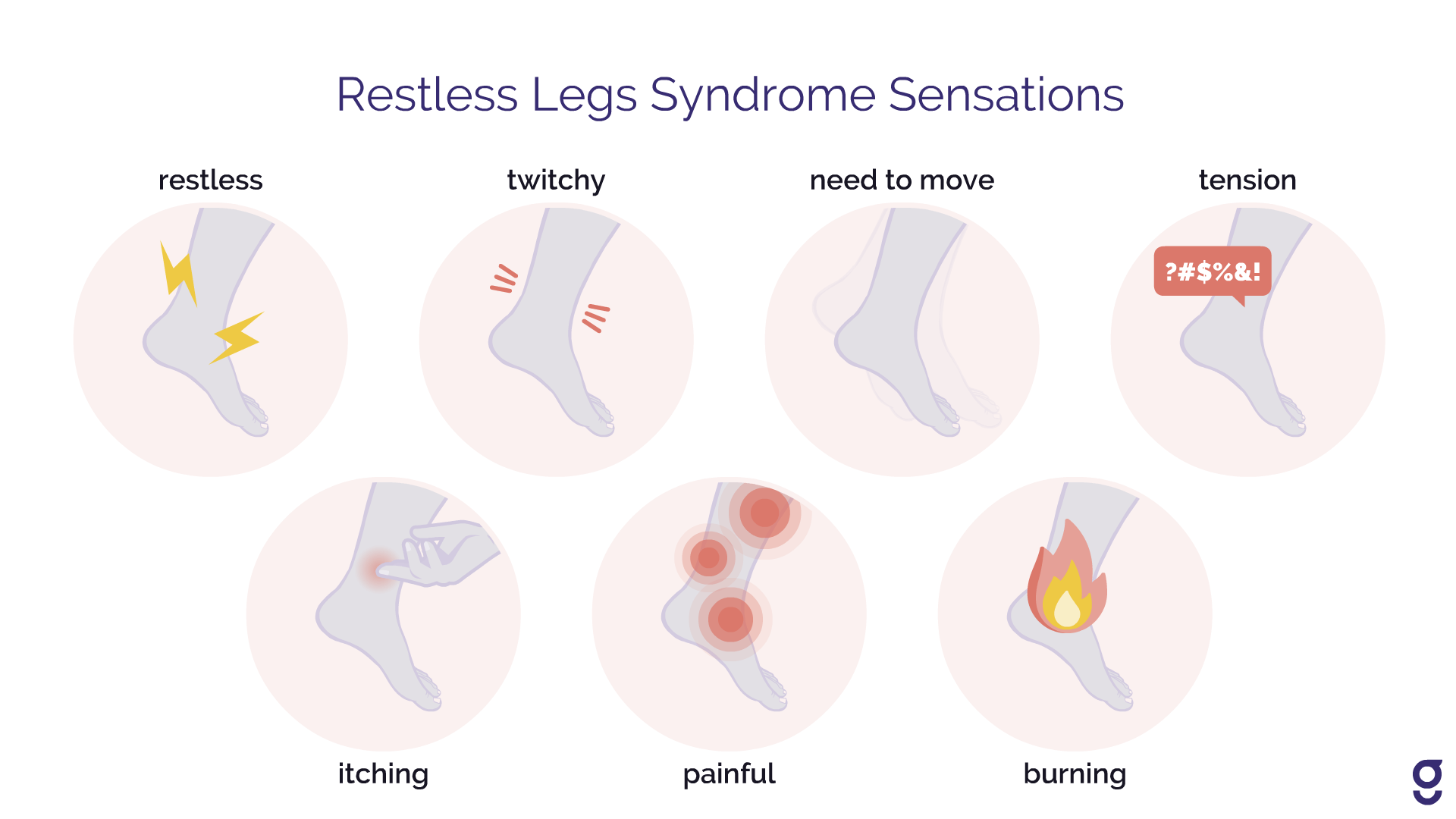
Symptoms of Restless Leg Syndrome
Common symptoms and how they affect patients
The hallmark symptom of RLS is an uncomfortable sensation in the legs, often described as a creeping, crawling, or itching feeling. This sensation typically occurs at rest and is temporarily relieved by movement. Many RLS sufferers also experience involuntary leg movements during sleep, known as periodic limb movements of sleep (PLMS). These symptoms can cause significant discomfort and disrupt sleep, leading to daytime fatigue and reduced quality of life.
How symptoms vary from mild to severe
The severity of RLS symptoms can vary greatly among individuals. Some people may only experience occasional discomfort, while others may have more pronounced and frequent symptoms. The intensity of symptoms can also fluctuate throughout the day, with many individuals reporting worse symptoms in the evening and nighttime. It is important to recognize the wide range of symptom severity and tailor treatment accordingly.
Impact of symptoms on daily life and sleep quality
RLS symptoms can have a profound impact on a person’s daily life and sleep quality. The discomfort and urge to move the legs can make it challenging to sit still for long periods, leading to difficulties in activities such as working, traveling, or even enjoying leisure activities. Sleep disturbances caused by RLS can result in significant daytime sleepiness, irritability, and impaired cognitive function. It is crucial to address these symptoms to improve overall well-being and quality of life.
This image is property of my.clevelandclinic.org.
Causes of Restless Leg Syndrome
Genetic Factors
Research has indicated a genetic component to RLS, with the condition often running in families. Specific gene variants related to the regulation of dopamine, a neurotransmitter involved in movement, have been identified as potential contributors to RLS development. However, more studies are needed to fully understand the genetic factors involved.
Neurological Causes
Dysfunction in the central nervous system, particularly in the areas of the brain that regulate movement and sensory processing, is believed to play a role in RLS. Imbalances in neurotransmitters such as dopamine and iron deficiency in these areas may contribute to the development of RLS symptoms.
Iron Deficiency and Other Nutritional/Mineral Causes
Iron deficiency is a well-known risk factor for RLS. Low levels of iron in the brain can disrupt the production and regulation of dopamine, leading to RLS symptoms. Other nutritional deficiencies, such as folate and magnesium, have also been implicated in RLS development. Proper nutrition and ensuring adequate levels of these minerals may help alleviate symptoms in some cases.
Pregnancy-Related Causes
Pregnancy is a time when hormonal and physiological changes can trigger or exacerbate RLS symptoms. The exact mechanisms are not fully understood, but hormonal fluctuations, increased blood volume, and nutritional demands may all contribute to RLS during pregnancy. These symptoms typically improve or resolve after childbirth.
Chronic Diseases as Potential Causes
Certain chronic medical conditions, such as kidney disease, diabetes, and peripheral neuropathy, have been associated with an increased risk of developing RLS. The underlying mechanisms linking these conditions to RLS are still being studied, but it is essential to recognize and address any underlying medical conditions to effectively manage RLS symptoms.
Risk Factors
Age-related risks
As mentioned earlier, RLS prevalence tends to increase with age. Older adults are more likely to develop RLS, and the severity of their symptoms may also be greater. Age-related changes in the brain and nervous system, as well as other medical conditions commonly seen in older adults, may contribute to the increased risk.
Family history and genetics
A family history of RLS is a significant risk factor for developing the condition. Having a first-degree relative, such as a parent or sibling, with RLS increases the likelihood of developing RLS compared to those without a family history.
Lifestyle factors and their impacts
Certain lifestyle factors have been associated with an increased risk of RLS. These include obesity, sedentary behavior, smoking, and excessive alcohol or caffeine consumption. Adopting a healthy lifestyle, including regular exercise and a balanced diet, may help reduce the risk of developing RLS or alleviate symptoms in those already affected.
Associations with other medical conditions
RLS has been found to be more prevalent in individuals with certain medical conditions, such as diabetes, kidney disease, and iron deficiency anemia. It is crucial for healthcare providers to assess and manage any underlying medical conditions to effectively treat RLS.
This image is property of www.cvmus.com.
Diagnosing Restless Leg Syndrome
Clinical evaluation and medical history
Diagnosing RLS begins with a thorough clinical evaluation and medical history assessment. The healthcare provider will ask about the nature and frequency of symptoms, their impact on daily life and sleep, and any known risk factors or underlying medical conditions. This information helps establish a baseline for further evaluation and treatment.
Physical and neurological examination
A physical examination may be conducted to rule out other potential causes of leg discomfort or movement abnormalities. Additionally, a neurological examination may be performed to assess sensory and motor function, evaluate reflexes, and identify any signs of nerve damage or other neurological conditions.
Role of sleep studies in RLS diagnosis
In some cases, a sleep study may be recommended to confirm the presence of RLS and determine the severity of associated sleep disturbances. A sleep study involves monitoring various physiological parameters, such as brain activity, oxygen levels, and leg movements, during sleep. This objective data can provide valuable insights into the nature and impact of RLS on sleep quality.
Differential diagnosis: Separating RLS from other conditions
It is essential to differentiate RLS from other conditions that may present with similar symptoms. Conditions such as peripheral neuropathy, arthritis, varicose veins, and nerve entrapment syndromes can all cause leg discomfort. By ruling out these conditions and identifying the specific characteristics of RLS, healthcare providers can make an accurate diagnosis and develop an appropriate treatment plan.
Treatment and Management
First-line treatments and lifestyle modifications
The first-line treatment for RLS typically involves lifestyle modifications aimed at alleviating symptoms and improving sleep quality. These may include regular exercise, maintaining a consistent sleep schedule, practicing relaxation techniques, and avoiding or reducing the consumption of caffeine and alcohol. Establishing a comfortable sleep environment and practicing good sleep hygiene are also important.
Prescription medications used in treatment
In cases where lifestyle modifications alone are insufficient to manage RLS symptoms, medication may be prescribed. Dopaminergic agents, such as pramipexole and ropinirole, are commonly used to reduce the sensations and urge to move associated with RLS. Other medications, including opioids, benzodiazepines, and anticonvulsants, may be considered for individuals with more severe symptoms or for those who do not respond well to dopaminergic agents.
Iron supplementation and dietary considerations
For individuals with RLS and iron deficiency, iron supplementation may be recommended. Increasing iron levels can help support dopamine production and alleviate RLS symptoms. However, iron supplementation should be done under medical supervision to avoid iron overload, as excess iron can be harmful. Additionally, maintaining a balanced diet that includes foods rich in iron, folate, and magnesium may also be beneficial.
Physical and occupational therapy
Physical and occupational therapy approaches may be used as part of a comprehensive treatment plan for RLS. Physical therapy can help improve muscle strength, flexibility, and circulation, reducing discomfort and improving symptoms. Occupational therapy can provide guidance on adapting daily activities to minimize symptom exacerbation and improve overall function.
Emerging treatments and therapies
Research into alternative treatments and therapies for RLS is ongoing. Some promising approaches include brain stimulation techniques, such as transcranial magnetic stimulation, and non-pharmacological interventions, such as pneumatic compression devices and transcutaneous electrical nerve stimulation. These emerging treatments show potential for effectively managing RLS symptoms and may be considered for individuals who do not respond well to traditional approaches.
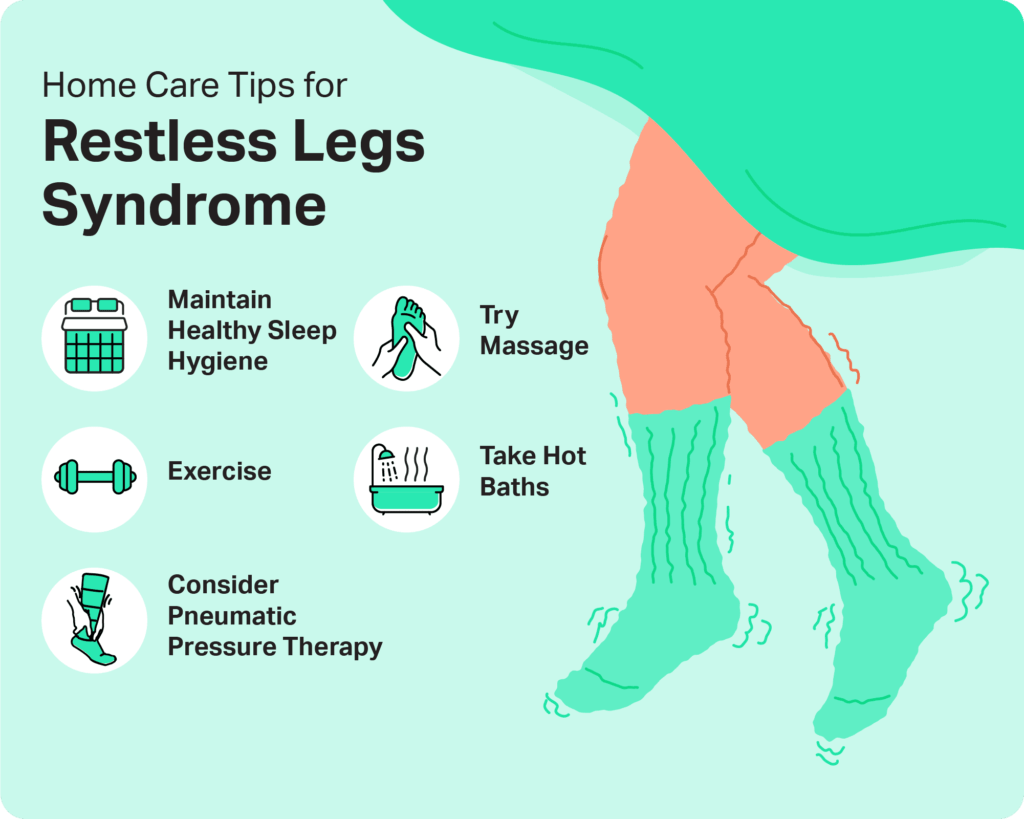
This image is property of www.cvmus.com.
Lifestyle Modifications and Home Remedies
Exercise and relaxation techniques
Regular exercise can help reduce RLS symptoms by promoting circulation, reducing stress, and improving sleep quality. Low-impact activities such as walking, swimming, or cycling are often recommended. Relaxation techniques, such as deep breathing exercises or progressive muscle relaxation, can also help alleviate symptoms and promote a sense of calm.
Sleep hygiene for RLS sufferers
Establishing good sleep hygiene practices is crucial for individuals with RLS to improve sleep quality. This may involve creating a consistent sleep schedule, optimizing the sleep environment by ensuring a comfortable temperature, minimizing noise and light, and using relaxation techniques before bed. Avoiding stimulating activities, such as using electronic devices or consuming caffeine, close to bedtime is also important.
Avoiding triggers and managing symptoms at home
Identifying and avoiding triggers that worsen RLS symptoms can help individuals manage their condition effectively. Common triggers include stress, certain medications, and excessive use of alcohol or caffeine. Creating a relaxing bedtime routine and engaging in activities that promote calmness, such as reading or taking a warm bath, can also help manage symptoms at home.
Nutritional tips and supplements
Maintaining a balanced diet that includes foods rich in iron, folate, and magnesium is recommended for individuals with RLS. Foods such as lean meats, fish, leafy greens, nuts, and seeds can provide essential nutrients that support overall health and may help alleviate RLS symptoms. If necessary, dietary supplements can be considered, but it is best to consult with a healthcare provider before starting any supplementation regimen.
Medications for Restless Leg Syndrome
Understanding Dopaminergic agents
Dopaminergic agents are commonly prescribed to manage RLS symptoms. These medications work by increasing the levels of dopamine in the brain, thus reducing the sensations and urge to move associated with RLS. They can provide significant relief for many individuals, but they may also have side effects or lose effectiveness over time. Regular monitoring and adjustments by a healthcare provider are essential to achieve optimal symptom control.
Use of Benzodiazepines and opioids
In some cases, benzodiazepines or opioids may be prescribed to manage moderate to severe RLS symptoms. These medications can help improve sleep quality and decrease the discomfort associated with RLS. However, they carry significant risks, including the potential for dependence, tolerance, and other side effects. Their use should be carefully monitored and limited to individuals who have not responded well to other treatment options.
Anticonvulsants for symptom management
Certain anticonvulsant medications, such as gabapentin and pregabalin, may be used to manage RLS symptoms, particularly in individuals who do not tolerate or respond to dopaminergic agents. These medications work by modulating the electrical activity in the brain and reducing nerve excitability. They can provide relief for some individuals and may be used alone or in combination with other treatments.
Side effects and monitoring of medication use
It is important to be aware of the potential side effects associated with the use of RLS medications. Common side effects may include nausea, dizziness, daytime sleepiness, and cognitive impairment. Regular monitoring and communication with a healthcare provider are essential to assess the effectiveness of the medication and adjust the dosage as needed.
This image is property of www.medicoverhospitals.in.
Alternative Therapies
Acupuncture and acupressure
Acupuncture and acupressure are alternative therapies that involve stimulating specific points on the body to promote balance and alleviate symptoms. While research on their effectiveness for RLS is limited, some individuals may find these therapies helpful in reducing the severity of symptoms and promoting relaxation.
Massage therapy
Massage therapy can help relax tense muscles and improve circulation, potentially reducing RLS symptoms. It can also provide a sense of overall well-being and relaxation, promoting better sleep quality. Consult with a licensed massage therapist experienced in working with individuals with RLS to maximize the benefits.
Cognitive Behavioral Therapy (CBT)
Cognitive Behavioral Therapy (CBT) is a therapeutic approach that focuses on changing negative thought patterns and behaviors associated with a specific condition. In the context of RLS, CBT can help individuals develop coping strategies, manage stress, and improve sleep hygiene. CBT has been shown to be effective in reducing RLS symptoms and improving overall well-being.
Yoga and meditation as complementary treatments
Yoga and meditation practices can promote relaxation, reduce stress, and improve sleep quality. Engaging in gentle yoga poses and practicing mindfulness meditation can help individuals with RLS find relief from symptoms and promote a sense of calm and well-being. It is important to consult with a qualified instructor or therapist experienced in working with individuals with RLS to ensure safe and effective practice.
Living with Restless Leg Syndrome
Coping strategies for patients and families
Living with RLS can be challenging, but there are strategies that can help individuals cope with their symptoms. Seeking support from healthcare professionals, joining support groups, and connecting with others who have RLS can provide valuable emotional support and practical advice. Engaging in stress-reducing activities, maintaining a healthy lifestyle, and practicing self-care can also help individuals manage their condition and improve overall well-being.
Maintaining quality of life with RLS
While RLS can significantly impact an individual’s quality of life, there are steps that can be taken to minimize its effects. By implementing a combination of lifestyle modifications, adhering to prescribed treatments, and seeking appropriate support, individuals with RLS can achieve a better quality of life. It is important to remember that each person’s experience with RLS is unique, and finding individualized strategies that work best for them is key.
Support groups and resources
Support groups and resources dedicated to RLS can provide valuable information, advice, and emotional support for individuals and their families. These groups often offer a platform for sharing experiences, discussing treatment options, and connecting with others who understand the challenges of living with RLS. Exploring local and online support groups can help individuals find the necessary support and encouragement.
Long-term management strategies
Managing RLS is usually a lifelong journey. As the condition may change or evolve over time, it is essential to continuously assess and adjust the treatment plan. Regular communication with healthcare providers and staying informed about new developments in RLS research can ensure that individuals have access to the most up-to-date treatment options and strategies. With the right support and management strategies, individuals with RLS can lead fulfilling and productive lives.
This image is property of www.sleepfoundation.org.