Cures for Narcolepsy: A Comprehensive Approach to Restful Sleep
Are you struggling with sleep disorders and looking for a comprehensive solution? Look no further than Vector Sleep Clinic. Conveniently located in the heart of Rego Park and easily accessible from all 5 boroughs, our clinic is committed to helping you discover the power of uninterrupted sleep. We understand the negative impact sleep disorders can have on your health and productivity, which is why we offer a comprehensive approach to diagnosing and treating a variety of sleep disorders. Don’t let sleep disorders like narcolepsy hold you back from living your best life. Trust Vector Sleep Clinic for reliable and trustworthy care that will unlock the magic of restful nights where dreams meet rejuvenation.
This image is property of my.clevelandclinic.org.
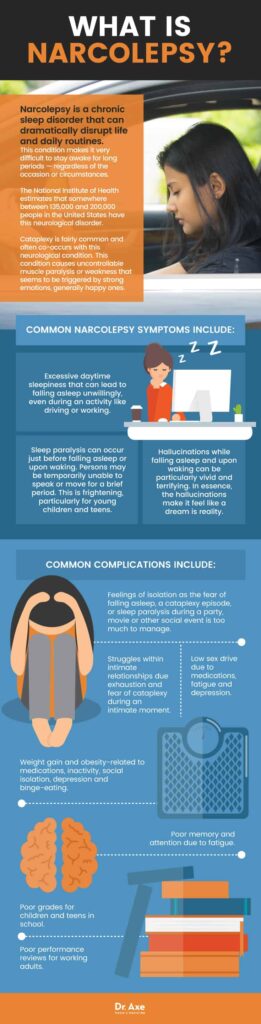
Understanding Narcolepsy
Definition and Symptoms
Narcolepsy is a neurological disorder that affects the brain’s ability to regulate sleep-wake cycles. Individuals with narcolepsy experience excessive daytime sleepiness, sudden attacks of sleep or “sleep attacks,” and a loss of muscle tone known as cataplexy. Other common symptoms include sleep paralysis, hallucinations, and fragmented nighttime sleep.
Causes of Narcolepsy
While the exact cause of narcolepsy is still not fully understood, it is believed to be linked to a combination of genetic and environmental factors. Research suggests that narcolepsy may be caused by a deficiency of hypocretin, a chemical in the brain that regulates sleep-wake cycles. Additionally, certain autoimmune reactions and brain abnormalities have been associated with the development of narcolepsy.
Types of Narcolepsy: Type 1 vs Type 2
There are two main types of narcolepsy: type 1 and type 2. Type 1 narcolepsy, also known as narcolepsy with cataplexy, is characterized by the presence of cataplexy and a low level of hypocretin in the cerebrospinal fluid. Type 2 narcolepsy, on the other hand, does not involve cataplexy and has normal hypocretin levels. Both types can significantly impact an individual’s daily life and require appropriate management.
Impact of Narcolepsy on Daily Life
Living with narcolepsy can be challenging, as the condition can significantly impact various aspects of daily life. Excessive daytime sleepiness can make it difficult to stay awake during work or school, affecting productivity and performance. Narcolepsy can also lead to social isolation, as individuals may avoid social activities due to the embarrassment or fear of falling asleep in public. It is essential to understand and address these challenges to effectively manage narcolepsy.
Diagnosing Narcolepsy
Importance of Accurate Diagnosis
Accurate diagnosis of narcolepsy is crucial to ensure appropriate treatment and management. Many individuals with narcolepsy go undiagnosed or misdiagnosed for years, leading to unnecessary suffering and misunderstanding of their symptoms. A proper diagnosis allows individuals to access the necessary support, education, and treatment options, enabling them to lead a better quality of life.
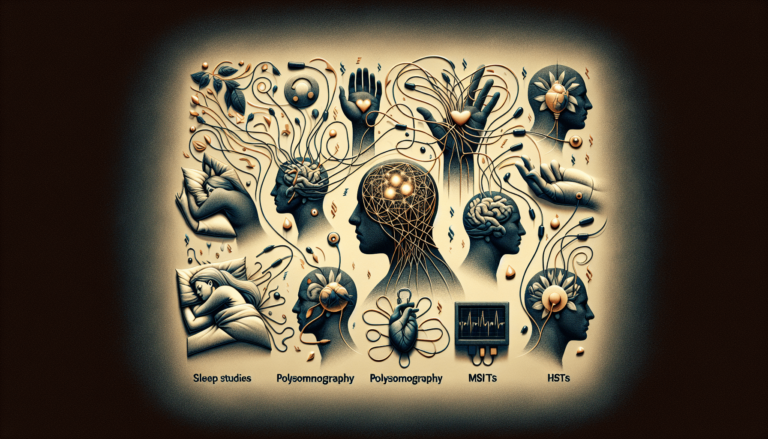
Overview of Sleep Studies
Sleep studies, also known as polysomnography, play a vital role in diagnosing narcolepsy. During a sleep study, you will be monitored overnight in a sleep clinic, where various measurements are taken, including brain activity, eye movements, muscle tone, and heart rate. This data helps sleep specialists evaluate your sleep architecture and identify any abnormal patterns or disruptions that may indicate narcolepsy or other sleep disorders.
Other Diagnostic Methods and Tools
In addition to sleep studies, medical professionals may use other diagnostic methods and tools to confirm a narcolepsy diagnosis. These can include multiple sleep latency tests (MSLT), which measure your tendency to fall asleep and enter rapid eye movement (REM) sleep during daytime naps, as well as assessing your medical history and conducting physical examinations. These comprehensive approaches ensure accurate and thorough evaluation.
Interpreting the Results
Once the diagnostic tests are complete, a sleep specialist will review the results to determine if you meet the criteria for a narcolepsy diagnosis. They will consider factors such as the frequency and severity of your symptoms, the presence of cataplexy, and the results from the sleep studies and other diagnostic methods used. It is essential to work closely with your healthcare provider to ensure an accurate interpretation of the results and a proper diagnosis.
Lifestyle Adjustments for Managing Narcolepsy
Sleep Hygiene Best Practices
Maintaining good sleep hygiene is essential for managing narcolepsy. Establishing a consistent sleep schedule, creating a comfortable sleep environment, and practicing relaxation techniques before bedtime can help improve the quality of your sleep. Avoiding caffeine and stimulating activities close to bedtime and ensuring regular exposure to natural light during the day can also contribute to better sleep hygiene.
Dietary Considerations
Certain dietary considerations can help manage narcolepsy symptoms. It is recommended to avoid heavy meals and large amounts of carbohydrates, as these can increase drowsiness. On the other hand, including protein-rich foods in your diet, such as lean meats, fish, and legumes, can help promote wakefulness. Additionally, incorporating omega-3 fatty acids, found in fatty fish and flaxseeds, may have a protective effect against certain symptoms of narcolepsy.
Exercise and Physical Activity
Regular exercise and physical activity can play a significant role in managing narcolepsy. Engaging in moderate-intensity aerobic exercises, such as walking, swimming, or cycling, can help improve daytime alertness and reduce symptoms of fatigue. It is important to find a form of exercise that you enjoy and can incorporate into your daily routine to reap the benefits of physical activity.
Managing Work and Social Life
Living with narcolepsy may require adjustments in your work and social life to accommodate your symptoms. Communicating openly with your employer or school about your condition and exploring flexible work or study arrangements, such as modified schedules or remote work options, can help create a supportive environment. Additionally, building a strong support network of friends, family, and support groups can provide understanding and emotional support.
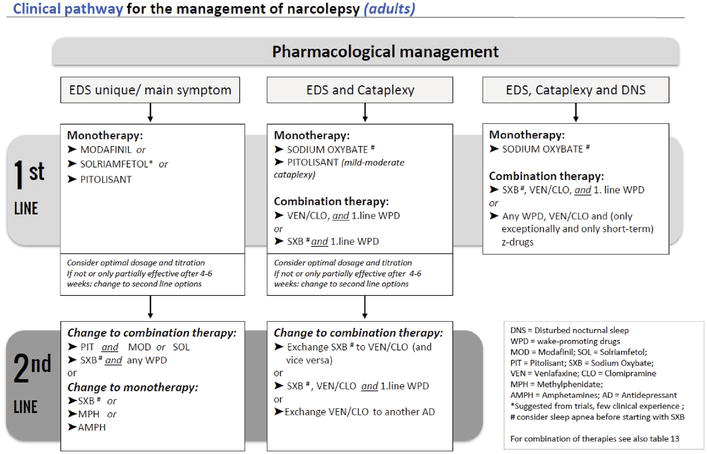
Pharmacological Treatments
Stimulant Medications
Stimulant medications are commonly prescribed to manage narcolepsy symptoms, particularly excessive daytime sleepiness. These medications work by stimulating the central nervous system and promoting wakefulness. They can help improve alertness, reduce sleep attacks, and enhance overall functioning. It is important to work closely with your healthcare provider to find the right medication and dosage for your specific needs.
Wakefulness-Promoting Agents
In addition to stimulant medications, wakefulness-promoting agents like modafinil and armodafinil are often prescribed for narcolepsy management. These medications are less likely to cause side effects commonly associated with stimulants, such as increased heart rate or agitation. They can help improve wakefulness and reduce excessive daytime sleepiness without interfering with nighttime sleep.
Antidepressants for Cataplexy
For individuals with narcolepsy accompanied by cataplexy, antidepressant medications, such as selective serotonin reuptake inhibitors (SSRIs) or serotonin-norepinephrine reuptake inhibitors (SNRIs), may be prescribed. These medications can help reduce the frequency and severity of cataplexy attacks by regulating brain chemicals involved in muscle control. It is important to discuss potential side effects and interactions with your healthcare provider.
Emerging Drug Therapies
Ongoing research in the field of narcolepsy has identified potential emerging drug therapies. These include medications that target the hypocretin deficiency underlying narcolepsy, aiming to restore normal sleep-wake regulation. While these therapies are still in development or clinical trials, they hold promise for future treatment options and may provide additional choices for individuals with narcolepsy.
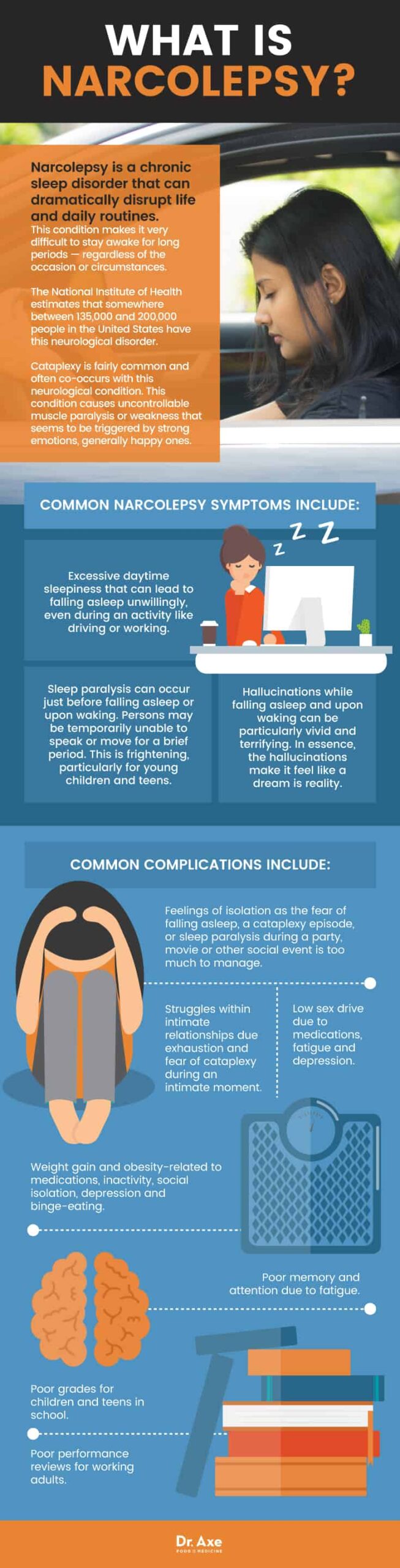
This image is property of draxe.com.
Non-pharmacological Therapies
Behavioral Therapy
Behavioral therapy, such as cognitive-behavioral therapy (CBT), can be beneficial in managing narcolepsy symptoms. This type of therapy focuses on changing negative thought patterns and behaviors that may contribute to sleep disturbances. CBT can help improve sleep quality, reduce anxiety related to sleep, and develop coping strategies for managing daytime sleepiness and other symptoms.
Scheduled Naps
Scheduled naps are a valuable tool for managing narcolepsy symptoms. Strategic planning of short naps throughout the day can help prevent excessive daytime sleepiness and combat sleep attacks. Napping at designated times can provide a much-needed energy boost and improve alertness. It is important to work with your healthcare provider to determine an appropriate nap schedule that suits your individual needs.
Light Therapy
Light therapy, also known as phototherapy, involves exposure to bright artificial light to regulate the sleep-wake cycle. This therapy can be particularly helpful for individuals with narcolepsy who experience disrupted circadian rhythms due to excessive daytime sleepiness. Light therapy sessions, typically performed in the morning, can help reset the internal body clock and promote wakefulness during the day.
Cognitive Behavioral Therapy for Insomnia (CBT-I)
For individuals with coexisting insomnia symptoms alongside narcolepsy, cognitive-behavioral therapy for insomnia (CBT-I) may be recommended. CBT-I focuses on addressing the underlying causes of insomnia and improving sleep quality. Techniques such as stimulus control, sleep restriction, and relaxation exercises can help individuals with narcolepsy establish healthier sleep patterns and reduce insomnia-related distress.
The Role of Technology
Wearable Sleep Trackers
Wearable sleep trackers have gained popularity in recent years as a tool for monitoring sleep patterns and identifying potential disruptions. These devices, typically worn on the wrist or placed under the mattress, track various sleep parameters such as sleep duration, sleep stages, and disruptions. While they may not provide a definitive diagnosis for narcolepsy, they can assist individuals in gaining insights into their sleep habits and aiding discussions with healthcare providers.
Smart Alarms
Smart alarms are an innovative technology that can assist individuals with narcolepsy in waking up at the optimal time during their sleep cycle. These alarms use data from sleep trackers to determine the most appropriate time within a preset window to wake the individual, ensuring they wake up feeling refreshed and alert. Smart alarms can help minimize the grogginess commonly associated with abrupt awakenings.
Sleep Apps for Managing Symptoms
Various sleep apps are available for smartphones and tablets, offering features such as relaxation exercises, guided meditation, and sleep tracking. These apps can provide individuals with narcolepsy access to practical tools for managing symptoms, promoting relaxation, and improving sleep quality. It is important to choose reputable, evidence-based apps and incorporate them into a comprehensive management plan.
Innovations in Narcolepsy Treatment
Advancements in technology continue to drive innovation in the field of narcolepsy treatment. Ongoing research aims to develop new therapies, including wearable devices that can detect and alert individuals to the onset of cataplexy or sleep attacks. These innovations hold promise for improving symptom management and enhancing the overall quality of life for individuals living with narcolepsy.
This image is property of www.uspharmacist.com.
Surgical Options and Considerations
Hypoglossal Nerve Stimulation
Hypoglossal nerve stimulation is a surgical treatment option for certain cases of narcolepsy with coexisting sleep apnea. This procedure involves the implantation of a device that helps stimulate the hypoglossal nerve, which controls the muscles of the tongue and airway. By stimulating these muscles during sleep, hypoglossal nerve stimulation can help reduce airway collapse and improve breathing.
Uvulopalatopharyngoplasty (UPPP)
Uvulopalatopharyngoplasty (UPPP) is a surgical procedure primarily used for the treatment of sleep apnea but may also be considered in specific narcolepsy cases with associated upper airway abnormalities. During UPPP, excess tissues in the throat, such as the uvula, soft palate, and pharynx, are surgically removed or repositioned to widen and stabilize the airway and reduce the risk of airway obstruction during sleep.
Tonsillectomy in Cases Related to Sleep Apnea
In cases of narcolepsy with coexisting sleep apnea and enlarged tonsils, a tonsillectomy may be recommended. Tonsillectomy involves the surgical removal of the tonsils, which can help alleviate airway obstruction and improve breathing during sleep. It is essential to consult with a healthcare professional to determine if tonsillectomy is a suitable option based on individual circumstances.
Risks and Benefits
Like any surgical procedure, surgical options for treating narcolepsy come with their own set of risks and benefits. It is important to thoroughly discuss these options with a healthcare provider, weighing the potential benefits of improved symptoms and better quality of life against the risks and potential side effects. Each individual’s situation is unique, and treatment decisions should be made in consultation with a qualified medical professional.
Alternative and Complementary Medicine
Herbal Supplements
Some individuals with narcolepsy may explore the use of herbal supplements as a complementary approach to symptom management. While research on the effectiveness of herbal supplements for narcolepsy is limited, certain natural products, such as valerian root, chamomile, and passionflower, are known for their calming and sleep-inducing properties. It is important to consult with a healthcare provider before incorporating any herbal supplements to ensure they are safe and appropriate for you.
Acupuncture
Acupuncture is an alternative therapy that involves the insertion of thin needles into specific points on the body to restore balance and promote overall well-being. Some individuals with narcolepsy may find acupuncture helpful in managing symptoms such as excessive daytime sleepiness, fatigue, and stress. However, it is important to consult with a licensed acupuncturist and inform them about your narcolepsy diagnosis before undergoing treatment.
Mindfulness and Meditation
Practices such as mindfulness and meditation can offer individuals with narcolepsy valuable tools for managing stress, promoting relaxation, and improving sleep quality. Mindfulness techniques involve paying attention to the present moment without judgment, while meditation focuses on cultivating a calm and focused state of mind. These practices can help individuals develop greater self-awareness and enhance their ability to cope with narcolepsy symptoms.
Yoga for Sleep Regulation
Yoga is a holistic practice that combines physical postures, breathing exercises, and meditation to promote overall wellness. Specific yoga poses, such as forward bends and restorative poses, can be beneficial for individuals with narcolepsy by promoting relaxation and reducing stress. Adding yoga to your daily routine can contribute to better sleep regulation and overall well-being.
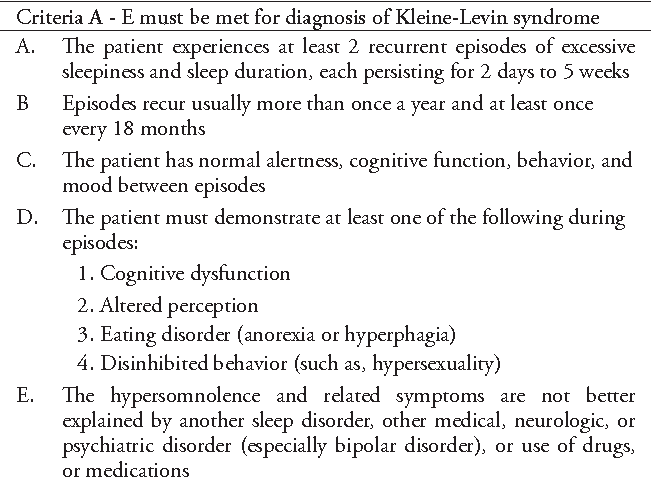
This image is property of cdnintech.com.
Support Systems and Communities
Family and Friend Support
Having a strong support system, consisting of family and friends, plays a crucial role in managing narcolepsy. Loved ones can provide understanding, empathy, and practical support on a daily basis. Educating those close to you about narcolepsy and its impact can foster a supportive environment where your needs are met, and your journey with narcolepsy is understood.
Online Forums and Support Groups
Online forums and support groups provide a valuable platform for individuals with narcolepsy to connect with others going through similar experiences. These online communities offer a safe space to share fears, challenges, and triumphs, and to seek advice or recommendations from others who understand the unique aspects of living with narcolepsy. Engaging with these communities can provide a sense of validation and support.
Working with a Sleep Specialist
Collaborating with a sleep specialist, such as a board-certified sleep medicine physician, can greatly assist in managing narcolepsy. Sleep specialists are trained in diagnosing and treating sleep disorders, including narcolepsy, and can provide guidance on treatment options and lifestyle adjustments. Regular check-ins and open communication with a sleep specialist can help ensure ongoing support and optimal management of your narcolepsy.
Educational Resources and Advocacy Groups
Educational resources and advocacy groups dedicated to narcolepsy play a vital role in providing information, raising awareness, and advocating for improved healthcare for individuals with the condition. These resources can provide up-to-date research, practical tips for managing symptoms, and opportunities to get involved in advocacy efforts. Utilizing these resources can empower individuals with narcolepsy to become active participants in their healthcare journey.
Conclusion: Embracing a Multifaceted Approach
Importance of Comprehensive Care
Narcolepsy management requires a comprehensive approach that encompasses various treatment options and lifestyle adjustments. Recognizing the multifaceted nature of the condition allows for a more holistic approach to address individual symptoms and improve overall well-being. A comprehensive care plan integrates pharmacological treatments, non-pharmacological therapies, support systems, and lifestyle adjustments tailored to each individual’s needs.
Combining Treatments for Optimal Outcomes
Combining different treatments, such as medication, behavioral therapy, and lifestyle adjustments, can often yield the best outcomes for individuals with narcolepsy. By working closely with healthcare providers and sleep specialists, you can develop a personalized treatment plan that optimizes symptom management and minimizes the impact of narcolepsy on your daily life. It is important to maintain open and ongoing communication to adapt the treatment plan as needed.
Adapting Strategies as Needed
Narcolepsy symptoms can vary in severity and may change over time. Therefore, it is essential to remain flexible and adaptable in your management strategies. Regularly reassessing your symptoms, discussing any changes with your healthcare provider, and being open to exploring new approaches can help ensure that your treatment plan remains effective as your needs evolve.
Empowerment Through Knowledge and Support
Empowering yourself through knowledge and seeking support is key to effectively managing narcolepsy. Educating yourself about the condition, staying informed about the latest developments in narcolepsy research and treatment, and actively engaging with support systems and communities can help you navigate the challenges of living with narcolepsy and improve your overall quality of life. Remember, you are not alone, and there are resources available to support you every step of the way.
This image is property of draxe.com.